Among the diseases of the musculoskeletal system, osteoarthrosis is a frequency leader.It is believed that the vast majority of the population of the planet at the age of 60 has the initial signs of changes in joint cartilage, and 14% already have manifestations of osteoarthrosis.The most common version of this disease is the osteoarthrosis of the knee joints.
Even so, "osteoarthritis" or "arthritis"?
Do not mix these two concepts.Arthrosis is the process of changing mainly the structure of the joints, and arthritis is an inflammation that could occur both in the context of the "intact" structure and in the context of osteoarthritis.
Changes in bone with osteoarthritis can be compared, for example, with growing growths in a tree trunk, which grows near the concrete fence and exerts pressure on this close with all its weight.
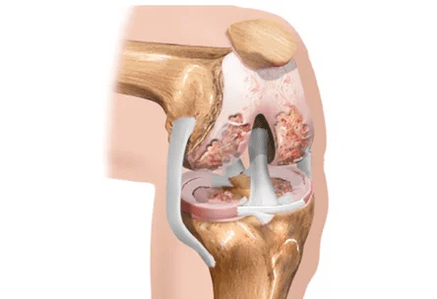
Normally, the surface of the bones in front of the others is separated by two layers of cartilage and mensures (additional cartilaginous plates).In addition to the "shock absorber" paper between the bones, the cartilage provides the landslide and mechanical correspondence with each other.Meniscus, which, due to large or small (but frequent) injuries, and also loses its elasticity, can be completely or partially further broken.
With age, and especially in the presence of a hereditary predisposition, the joint cartilage is thinner.That is why the bones of the hips and the bottom of the legs, which make up the knee joint for their purposes, are approaching dangerously with each other, can even arise friction between them.
Usually, in parallel with the thinning of the cartilage over the years, another unpleasant event occurs: the amount of intra -articular fluid decreases.This liquid is not just a purely mechanical "lubrication" of the joint from the inside.Provides bone, meniscus and joint cartilage nutrition.The violation of the "supply" of all these structures is a real disaster for the articulation!
If there is a physical overload of the joint, then bone growth appears on the surfaces of the bones and begin to grow, more similar to the points or peaks.For the knee joint, such overloads will be weightlifting (including overweight of your own body!), Physical work with emphasis on the knees (for example, eliminating the garden), walking constantly on the stairs, running, wearing uncomfortable shoes, flat feet and many others.Now it is easy to imagine what is happening within the knee joint during the development of osteoarthritis and how it manifests itself.
How does the articulation work?
Each of us has seen the articulation cartilage many times at the end, for example, chicken bone.It covers small areas of contact with the bones.Under the joint cartilage there is a subchondral or perized bone.The human musculoskeletal system is organized similarly.
The majority of the person's joints consist of bones, synovial shell (articular) and intra -articular fluid.
What happens to the articulation with osteoarthritis?
Under the influence of all those charges that have already been mentioned, there is a compaction and growth of the thin bone, as a result, a greater trauma of the articular cartilage.
Products of the cartridge of the cartilage formed due to microtrauma fall into the synovial fluid.It is so fixed by nature that they are strange substances for synovial shell and cause inflammation.Synovial fluid formation is altered, which is generally a kind of "transporter", similar to a continuous cycle of blood enrichment and purification.In addition, joint liquid becomes less than hyaluronic acid.It is worth counting on this acid.
Hyaluronic acid provides the viscosity of the synovial fluid, creates the "effect of the buffer" and the "lubrication effect" between the bones, reducing its friction with each other.It is thanks to this substance that the articular fluid in consistency resembles the protein of the egg, not to the water.Another important role of hyaluronic acid is to guarantee the supply of nutrients from the joint liquid deeply in the joint cartilage, since there is no place to carry it: the blood vessels are not directly suitable for the cartilage.In the same way, the "spent" substances of the cartilage are eliminated in the joint fluid: using hyaluronic acid molecules.
Therefore, an improved bone seal occurs and unbearable conditions for joint cartilage are created.
The cartilage receives a signal to adapt to these extreme conditions, and its change begins, otherwise it is called remodeling.This is mainly manifested by a decrease in the elasticity of the cartilage.
In the late stage of the development of osteoarthritis, the bone becomes rigid, but at the same time more fragile, the cartilage itself is partially impregnated with calcified calcium.
Symptoms
The development of osteoarthritis begins with a slight knee pain, appearing after walking the stairs, physical activity, walking on foot.Such mild pain can appear for several months, or even years.Then they become more pronounced.In the initial stage of disease development, knee bones are not deformed, but a slight swelling of the joint itself can be observed.
In the second stage of the development of the disease, pain becomes more intense and occurs after a slight load.In addition to pain, a crunch appears in the knee joint, which differs from the usual soft abuse of a healthy joint with pain.In addition, the deformation of the joint becomes remarkable, the bones to the touch become broader and more rude.Linding the knee more than 90 degrees becomes problematic.
In the third stage of the disease, knee pain becomes severe and constant, not even passing even in the rest period.Knee mobility becomes minimal, it often does not bend more than 90 degrees and does not extend until the end.The deformation of the joint bones becomes so strong that there is a curvature of valgo (in the form of x) or variability (in the form of O) of the legs.
Diagnosis
Inspection

In the early stages of the disease, the articulation does not change, mobile, the muscles around it are preserved and strong enough.Only by palpation (pressure) of certain points, more often on the internal surface of the joint, the local (local) pain is determined.The doctor asks the patient to perform several squats, bend, straighten the leg in the knee, place the face on the couch and conduct flexion-expansions (this is called "passive" movements).In this case, in addition to pain and limiting the volume of movements, you can determine the crunch, by clicking on the joints.With a pronounced inflammatory component, the joint increases in size, it seems that it is "pumped" with liquid.With a distant range process, knee flexion can be partial or completely absent, when examined, the surface of the joint seems uneven, tuberous, the limb can be curved (displacement of the axis of the limb, "conjured").
Laboratory and Instrumental Research
- The mandatory laboratory surveys program includesGeneral, biochemical and immunological blood analysis, urine analysis.In the general blood analysis, attention will be paid: the highest level of leukocytes and the highest erythrocyte settlement rate, indicating inflammation.In the biochemical analysis of blood, metabolic metabolic indicators are important, the level of "liver" enzymes.In the immune analysis, the presence or absence of signs of systemic inflammation will be determined, this is evidenced by the level of C -reactive protein.Urine analysis will reveal the "sand" content - uric acid crystals.
- Synovial Fluid Analysis (joint)It is prescribed in the event that this liquid is in sufficient quantities.That is, when the joint is swollen, swollen.In conditions of compliance with sterility, the doctor drills the articular capsule in a strictly defined place, inserts the needle into the joint cavity and then eliminates excess fluid.Part of the material obtained enters the laboratory for analysis.At the end of the procedure, the anti -inflammatory drug of the glycocorticoid group is more frequently administered in the joint cavity (for example, Diprospan).
 radiography.An image of both knee joints is mandatory, this is necessary to compare a sick knee with a healthy.In the image, attention is paid to the width of the joint gap (it is judged by the state of meniscus and cartilage), the presence or absence of bone spikes-osteophytes, signs of destruction (destruction) of bones.
radiography.An image of both knee joints is mandatory, this is necessary to compare a sick knee with a healthy.In the image, attention is paid to the width of the joint gap (it is judged by the state of meniscus and cartilage), the presence or absence of bone spikes-osteophytes, signs of destruction (destruction) of bones.- Ultrasound of knee jointsYou will answer questions about the preservation of the meniscus, the presence of a baker cyst, the severity of inflammation, the presence or absence of uric acid crystals (in the presence of gout).
- MRI (magnetic resonance image).This study is prescribed if an ultrasound does not give an exhaustive answer to the questions of a specialist.Magnetic resonance is mandatory for those patients who plan to perform arthroscopy.
- Arthroscopy.It allows you to visualize, that is, personally evaluate the condition of the articulation.The method is indispensable for controversial diagnoses, suspicion of traumatic damage of meniscus and ligaments (then directly during the study, it is possible to quickly eliminate the means or torn ligaments).
Treatment of knee joint osteoarthritis
The principles of integral treatment must be followed, which include:
- Detailed consciousness of the patient about the disease
- The use of physiotherapy exercises, which includes: Specific exercises for joints in a lie position, swimming
- Maintain optimal body weight
- Use an orthosis (soft bandage or at least one elastic bandage) during an augmented load in the joint, on the road, during a walk, etc.
- Non -physical methods (physiotherapy).This type of treatment offers excellent results with precision with the osteoarthritis of the knee joint (gonarrosis).Apparently, this is due to the fact that the joint is available for the influence of factors such as magnetic and laser radiation.To treat the knee joint, you can use magnetic currents, UHF, cryio -exposition (translated from Greek means the effect of cold).Physiotherapeutic procedures are widespread, treatment courses are usually brief, 10, maximum daily sessions or every two days.It should only be remembered about possible contraindications, which include tumor processes, diseases of the thyroid gland and pelvic organs, as well as systemic inflammatory diseases (autoimmune).
- Pharmacological therapy.

Principles of osteoarthritis therapy:
- Relieve pain
- delay the additional destruction of joint structures
- Restore the loss articular function.
Non -steroidal anti -inflammatory drugs
For pain relief, NCON -Drug Drugs are used.They are used in and in the form of applications (skin application).Applications (local therapy) are a very effective method, especially when it comes to the early stages of the disease.Before using a gel or cream that contains NSAIDs, it is necessary to make sure there are no skin changes, whether erupting, pustules or cracks.The general rule of local treatment is to use the selected cream or gel at least twice a day, and if unpleasant sensations arise, to cancel the complete disappearance of these manifestations.Intramuscular administration of analgesics is not currently recommended, since the risk of side effects as a result of the administration using a syringe does not decrease, but rather the opposite.In the case of pronounced inflammation, the accumulation of a large number of intra -articular glucocortic drugs is allowed, but it should be taken into account that this procedure must be carried out no more than 1 time every 3 months.
Condroprotectors
A greater anti -inflammatory effect of "step" with osteoarthritis are preparations of chondroitin or glucosamine.They, like NSAIDs, fight with inflammation at the level of decent joint structures, but have less side effects and, most importantly, retain their anti -inflammatory effect several months after cancellation.
Condroprotectors are a collective name for a group of medications that at the same time contain chondroitin and glucosamine sulfate: "construction bricks" of the cartilage.Despite the apparent high -cost treatment with condoprotectors, their convenience for patients and effectiveness is difficult to overestimate.First, these substances, accepted inside, are perfectly absorbed from the stomach, and the losses of the medication "along the way" to the cartilage are minimal.Secondly, they can suppress inflammation in the joint and, in addition, they reliably slow the process of destruction of the articular cartilage!Most of the time they are prescribed courses, because they have a quite long "AS" that lasts several months, and sometimes even up to six months.
Hyaluronic acid -based medications are qualified Hialuronates of SO.These funds are sold in the form of syringes prepared for intra -articular administration.Hialuronts are an artificial synovial fluid.The effect of treatment with this method can last up to 12 months.
Surgical treatment of the osteoarthritis of the knee joint
As with the osteoarthritis of the hip joints, in the case of serious changes and persistent loss of function, it occurs to the operation.With gonarrosis, two types of interventions are currently performed: arthrodesis (motionless compound) and endoprothetic.The first operation is rarely performed, according to special indications, when the installation of an endoprothesis is impossible for any reason.The result of this operation is that the knee becomes motionless.But it doesn't hurt.Endoprothetics operation is much more profitable in terms of function.Remember that with great body weight, this operation is not performed: the risk of complications in the postoperative period is too large.From the moment of the elimination of the damaged sections of the Board and the installation of the prosthesis until the function is completely restored, they do not spend more than three weeks.
How can we threaten ridiculous osteoarthrosis?
Over time, osteoarthrosis does not go back, but only aggravates, especially while maintaining provocative factors.Consider the main sources of danger to the health and life of a patient with osteoarthritis.
- Chronic pain of various intensity- A very important risk factor, especially in the elderly.Constantly experienced unpleasant sensations can lead to sleep alteration, a reduced mood and even depression fund.It is difficult to predict which chain of adverse events extract listed phenomena.
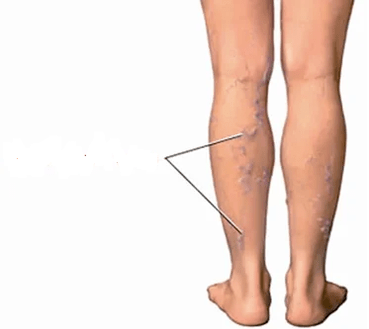
- VENAS PATHOLOGY.The constant inflammation in the knee area, the growth of spikes-osteophytes of bones, which can mechanically damage the popliteal vessels, can lead to the development or progression of the varicose veins of the legs of the legs.Sometimes, orthopedists refuse to operate their knees until varicose nodes are eliminated, but phlebologists (veins specialists) do not begin surgery in their veins until there are pronounced changes in the knee joints.
- Reduced limb function.With a distant scope process, the articulation can completely lose the ability to move, and this, in most cases, is a sign of disability.
- Participation of other joints.We have already discovered how such a common phenomenon, as flat feet, can "throw" the knee joint and lead to the development of osteoarthrosis.In the same way, throughout the chain, there is a participation in the painful process of the knee joint from the opposite side.If the patient neglects the recommendations, he refuses to use a cane, preferring to "limp on his two", the osteoarthritis of the hip joints develops very soon.The legs are twisted, the march becomes a "duck."
- immobility.This serious complication of the disease occurs in cases where the bones of the joint are destroyed very, there is no cartilage, the movement in the joint is very painful or impossible due to the fusion (this is called "ankylosis") of the bones with each other.In this situation, only surgery can help the patient, but only if it is technically feasible.Overcome is dangerous in the general sense: cause obesity, osteoporosis, muscular atrophy, the rapid development of diseases of internal organs.In addition, an immobilized person, of course, must be constantly taken care of.
- INOPERABILITY.Unfortunately, there are a number of states that make the operation impossible, and one of them is "careless" osteoarthritis from afar in patients older than 80 diseases with serious related diseases.
Prevention
- Exclude articular injuries.It seems: there is nothing easier.For a while, abandoning jumps, running, walking down the stairs, dance, high heels is not difficult.In practice, it turns out that it is this point that causes most protests by patients.A person, if he suffers recently, is generally not ready for the fact that some important point will be lost in his daily life.But if you do not follow these tips, there is the danger of a rapid decrease in the quality of life and disability.
- Reducing weight and keeping it within optimal limits is an extremely important recommendation!No matter how miraculous this effect or that tool has, fat people will not be able to appreciate it.Because while the joints are overweight, microtraumas are repeated daily.This can reduce all efforts to "no."In addition, for some treatment methods, obesity is a direct contraindication.
- Walk with support.The universal rule to download the joint using the support is this: a cane, a crutch or a handrail must be in the opposite hand to the affected limb.That is, if the right knee hurts, the cane must be kept on the left and vice versa.
- Correction of flat feet.It would seem, how can the flat feet be connected and the osteoarthritis of the knee joint?Results directly.If the foot is incorrectly installed (now we are talking about longitudinal or mixed flat feet, not on the transversal) the load is redistributed in the knee joint.In this case, the severity of the body with a step does not fall in the center of the joint, but to the right or to the left.Consequently, the right or left meniscus suffers more, and since it suffers more, we wear faster.Then comes the "tail" of the joint cartilage where the menisc cannot deal with its function.This process ends with the formation of typical "arthrose" changes with a typical side in the knee joint (the appearance of bone growth).





































